Types of Mastectomies for the Treatment of Breast Cancer
A Must Have for all affected by Lymphedema, Lipedema and related diseases. This new book focusing on the Self-Management of Lymphedema is specifically geared toward the patient, caregivers, and family members.

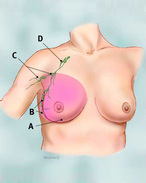
Sentinel Lymph Node
Lymphedema is a common side effect of mastectomies.
Mastectomies are alternatives to a lumpectomy, a breast-conserving surgery, in which only the tumor is removed from the breast.
Some women at very high risk of developing breast cancer may choose to have a mastectomy even when there is no sign of cancer in order to significantly reduce risk of developing breast cancer in the future. High risk is determined by a strong family history of breast cancer and/or the presence of certain genetic mutations (BRCA gene mutation) that increase the risk of breast cancer. A preventive (prophylactic) or risk-reducing mastectomy involves removing both breasts, also known as double, or bilateral mastectomy.
Types of Mastectomies:
Simple (or total) Mastectomy: A total mastectomy, also known as a simple mastectomy, involves the removal of the entire breast, including the breast tissue, areola and nipple. Muscle tissue and lymph nodes in the axilla (underarm area) are not removed during this procedure.
A sentinel lymph node biopsy (SLNB) may be done at the time of a total mastectomy; this is a procedure in which the sentinel lymph node (the first few nodes into which a tumor drains) is identified using blue dye (a radioactive substance), removed, and examined by a pathologist to determine whether cancer cells are present. If no cancer is present, no further lymph nodes need be removed. If cancer is found, the surgeon may remove additional lymph nodes, or suggest radiation to the area.
Total mastectomy is most appropriate for patients who have ductal carcinoma in situ (DCIS), or other underlying non-invasive breast cancer, advanced but localized breast cancer, or those who have a breast cancer recurrence. This procedure is also performed for women seeking prophylactic mastectomies.
Modified Radical Mastectomy: A modified radical mastectomy combines a simple mastectomy with the removal of the lymph nodes under the arm, known as axillary lymph node dissection. In this procedure, levels I and II of the axillary lymph nodes are removed (see image). Modified radical mastectomy is most appropriate for patients who have invasive breast cancer or inflammatory breast cancer. While the procedure is performed, the removed lymph nodes are examined to identify whether cancer cells may have spread beyond the breast.
Radical Mastectomy: During this most extensive type of surgery, the entire breast, nipple, axillary lymph nodes, nipple, areola and chest muscle wall is removed. In this procedure, levels I, II and III of the axillary lymph nodes are removed (see image). A radical mastectomy is most appropriate for patients who have extensive breast tumors, or if cancer cells have invaded the chest muscles. For many years, this was the standard surgery, but today it is rarely performed since modified radical mastectomies have proven to be just as effective and less disfiguring.
Partial Mastectomy: This is a breast-conserving surgery in which the surgeon removes only the tumor and the tissue around it. This procedure is often followed by 6 to 8 weeks of radiation therapy targeting the breast tissue. The radiation kills cancer cells and prevents them from spreading or recurring.
There are two forms of partial mastectomy: A lumpectomy removes the tumor and a small area of normal tissue surrounding the tumor.
a quadrantectomy removes the tumor and more of the breast tissue than a lumpectomy.
Skin-Sparing Mastectomy
This procedure involves removal of all the breast tissue, nipple and areola, however, most of the skin over the breast is left intact. The amount of breast tissue removed is the same as with a simple mastectomy, and implants or tissue from other parts of the body can be used during the surgery to reconstruct the breast immediately following the mastectomy.
Many women prefer skin-sparing mastectomy because it offers the advantage of less scar tissue and a reconstructed breast that seems more natural. It may not be a good method for tumors that are large, or near the skin surface.
Nipple-Sparing Mastectomy: A nipple-sparing mastectomy is a newer technique and a variation of the skin-sparing mastectomy.. During this procedure, the surgeon removes all the breast glandular tissue from underneath the skin, leaving the nipple and areola intact. A nipple-sparing mastectomy leaves fewer visible scars but is leaving behind more tissue than with other forms of mastectomy, which could result in a higher risk of cancer developing compared to other procedures. However, improvements in this surgical procedure have resulted in lowering this risk, and experts consider nipple-sparing mastectomy to be an acceptable treatment for breast cancer in properly selected women.
This form of mastectomy may be an option for women who have a small, early-stage cancer near the outer part of the breast, with no signs of cancer in the skin or near the nipple. Some women opt for this procedure if they are high risk for breast cancer and wish to prevent it from occurring.
Breast Reconstruction following Mastectomy: After having a mastectomy patients may opt to having the breast surgically reconstructed to restore the breast’s appearance. Although each case is different, most mastectomy patients can have reconstruction, which can be performed at the same time as the mastectomy or sometime later. Women considering reconstructive surgery should discuss this with the surgeon and a plastic surgeon prior to the mastectomy. This allows the surgeon to plan the treatment that is most appropriate.
Many women develop lymphedema following breast cancer surgery; it is of paramount importance to treat lymphedema correctly - in the publication "It's not just a Swelling - Lymphedema" patients learn all aspects of effective management of lymphedema.
This book is available on Amazon as hardcover, paperback, or E-book; it is also available on Lulu
Joachim Ernst Zuther
Lymphedema Blog
+1 772-913-1027
email us here
Visit us on social media:
Facebook
LinkedIn
Instagram
YouTube
Joachim Zuther, Lymphedema Specialist, talks about the Incidence of Lymphedema
Distribution channels: Beauty & Hair Care, Education, Healthcare & Pharmaceuticals Industry, Sports, Fitness & Recreation, World & Regional
Legal Disclaimer:
EIN Presswire provides this news content "as is" without warranty of any kind. We do not accept any responsibility or liability for the accuracy, content, images, videos, licenses, completeness, legality, or reliability of the information contained in this article. If you have any complaints or copyright issues related to this article, kindly contact the author above.
Submit your press release